
But always read them back before you submit them, as dictation is never 100% accurate!
#Soap notes full#
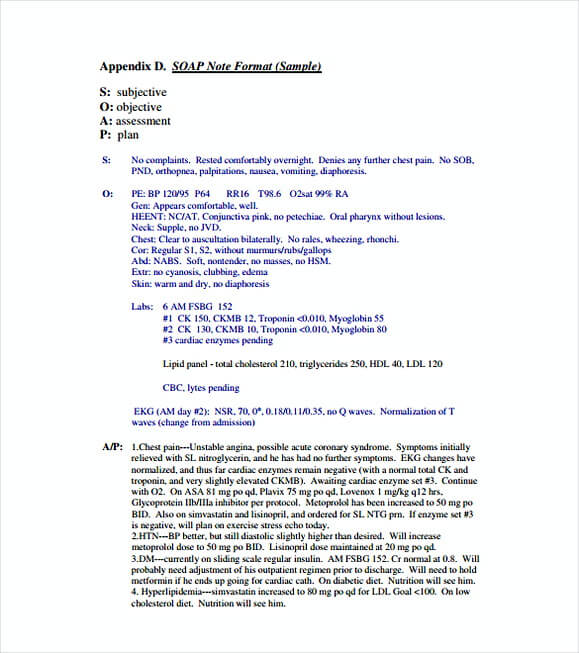
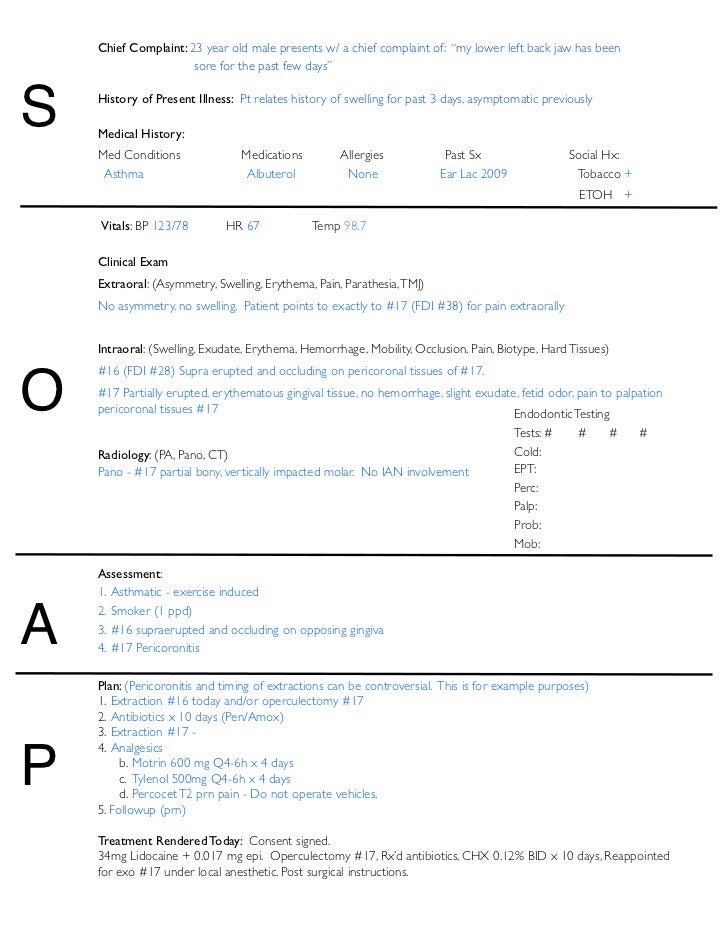
Note that in a patient’s initial evaluation, your plan should be more detailed, as you’re planning for a patient’s full course of treatment. Think of your plan entries in terms of goals-they should be measurable and include an approximate timeframe to achieve them. It should include steps to be taken in the patient’s course of treatment, such as future treatment recommendations or changes to an existing course. The Plan portion of your SOAP note looks forward. Be sure to make note of how the patient responded to this particular treatment and, if you’ve seen them previously, how they are progressing in their recovery. Here you’ll detail your overall findings, based on your prior evaluations and the treatment you’ve just provided. The Assessment section is completed immediately after the treatment has ended. As a massage therapist, you might observe characteristics such as posture, range of motion, or soft tissue tension. In a general clinical setting, that would include things like patient temperature or weight. The Objective entry consists of your impartial observations of the patient’s condition.
#Soap notes series#
The Zeel Provider App makes the Subjective entry easy by providing a series of evaluation tools to document the patient’s condition and symptoms. That could include an injury they’ve experienced, pain they are feeling, the severity of pain, and how it might be affecting other areas of their life, such as their sleep or ability to perform daily tasks.Īvoid adding your own assessments and interpretations to this section-this is the patient’s opportunity to tell his or her own story as they experience it. The Subjective entry consists of information the patient gives you. The Assessment and Plan portions are completed after a session has ended, since they contain information gathered during treatment, along with your future recommendations. You’re collecting information that will inform your therapeutic choices for the treatment you’re about to provide. The Subjective and Objective portions of an evaluation take place at the start of an appointment, before you’ve begun treatment. In some instances, you’ll also have a section detailing Treatment. SOAP stands for Subjective, Objective, Assessment, and Plan.

With Zeel you can complete your notes right in the Provider App. This easy-to-use system is designed to help you assess your patient’s unique needs, explain their treatment, and map out a care plan for achieving their recovery goals.

This documentation is also a crucial factor in health insurance processing-it helps ensure the patient will have their treatment covered by their plan.
SOAP notes completed for each appointment allow your patient’s care team (which includes you!) to better understand their condition and track their progress.įor future practitioners who work with your patient, your SOAP documentation can help inform their treatment choices and enhance the patient’s continuum of care. For providers taking appointments that are covered by patients’ insurance-such as medical massage or physical therapy-completing clinical documentation in the form of SOAP notes is a key component of the treatment process.


 0 kommentar(er)
0 kommentar(er)
